ACC Q Data Medical Billing
by ACC Q Data Medical Billing
Description
Medical billing is a transmission between the medical provider and the insurance company. The medical billing process/medical cycle is also known as Revenue cycle management. It includes billing, management, and payments of the claims. The billing invoices are known as claims.
The process begins when the practitioner diagnoses the patient and update the patient’s medical records. The practitioner adds a five-digit procedure code to the patient record, then it is transmitted to the insurance company. The insurance company reviews the claim and evaluate patient eligibility. Approved claims are reimbursed and denied claims are further appealed for reconsideration.
AccQdata plays an important role in the medical billing cycle. We work as a mediator between the provider and the insurance company. The medical billing cycle includes many steps, from insurance verification to denial management. We follow all these steps to bill the claims. We also inform our clients about the status of their claims by live reporting.
We are doing medical billing by completing various types of steps followed under the expert guidelines. Those steps involved Insurance Verification/ Authorization, Patient Demographic Entry, CPT & ICD Coding, Charge Entry, Claims Submission, Payment Posting, AR Follow-up, Denial Management, and Reporting.
Insurance Verification/ Authorization
It is necessary to complete insurance verification before a patient receives medical services. We verify patient insurance coverage on all primary and secondary payers and update patient accounts, so we verify that the required insurance criteria are correct or not.
Patient Demographic Entry
We verify all the patient insurance and demographic details completely before updating in the billing software. This helps physicians understand their patient's medical situations and recommend a certain course of action.
CPT & ICD Coding
CPT & ICD Code is a five-digit code used to describe the procedures, diagnoses, and aids a patient has received during their medical appointment. We review all claims before submission to verify if ICD-10 & HCPCS codes are valid or not.
Charge Entry
We assign every patient account with the appropriate $ value as per the coding and with an appropriate fee schedule. Patient accounts are assigned with the Charges entered will determine the reimbursements for the physician's service.
Claims Submission
Our team follows the medical billing claim submission process step by step such as payer services like member services, enrolment, provider credentialing, eligibility, claim administration, repricing transactions, adjudication, settlement EOB/EOP presentment.
Payment Posting
Our team identifies, manage and monitors the payment records of patients in the billing management software. They also classify the problematic areas and their reasons along with APT actions to be taken on resolving the issues.
AR Follow-up
Our AR team continues to follow up on all claims until they are paid proportionately. Our team is responsible for looking after denied claims and reopening them to receive maximum reimbursement from the insurance company.
Denial Management
We investigate every unpaid claim, uncover a trend by one or several insurance carriers, and appeal the rejection appropriately as per the appeals process in the provider contract. Also, we organize and identify errors before claims are submitted for payments.
Reporting
We collect and manage all medical data and show updated information on our client's dashboard. We report the live status of the claims so our clients can check the status of their claims.
AccQdata understands the full aspects of billing guidelines and we follow them exquisitely. We are expertise in workers' compensation. We help you to negotiate faster and provide consistent support. We also live report status of claims on a customized dashboard with daily updates. We collect data from our clients and manages them in our software. We collect data of patients via mail, email, dropbox, documents, and many other ways. Our experts organize that data in an ideal way that helps to build the process faster and smoother. We also plan weekly web meetings with our clients and discuss collections and resolving queries. We provide them a manageable work schedule. We identify and reduce billing errors by resolving them. By providing excellent services, we aim to provide our clients with exceptional medical billing solutions and empower them to achieve more.
For more information available at ACC Q Data Medical Billing
Related Websites
-
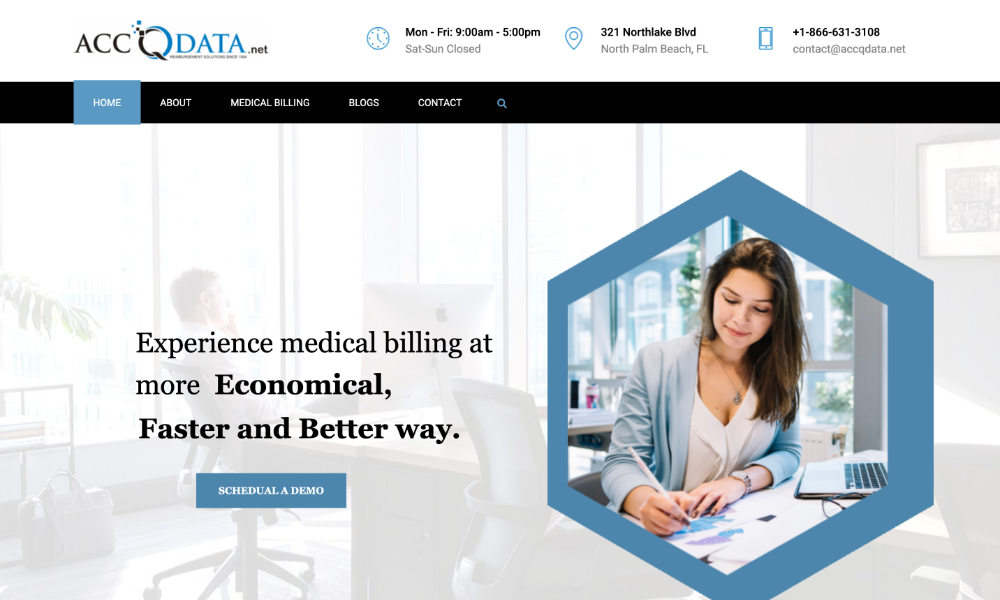
Gator Packaging
by Gator Packaging
868 -
Nirmal Web Studio
by Nirmal Web Studio
925 -
Aura Home Remodeling & Construction
by Aura Home Remodeling & COnstruction
731